Surgery for a spine tumor depends on the nature and location of the tumor.
Resection: When possible, the tumor is resected (removed) to relieve pressure and pain. This is delicate surgery, as tumors can be adjacent to important spine structures. At Weill Cornell Medicine, we emphasize intraoperative monitoring and stimulation of the spinal cord to maximize the safety of the resection.
Spine Stabilization: For metastatic spine tumors, we offer our patients state-of-the-art spinal stabilization to preserve mechanical and neurologic function and improve quality of life. We emphasize minimally invasive techniques, such as retropleural thoracotomies, short segment fusions, carbon fiber instrumentation, and the use of cages to enhance fusion.
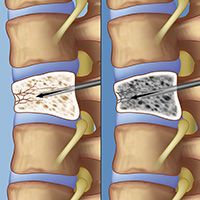
In a vertebroplasty, the surgeon advances a needle through the skin on a patient’s back under x-ray guidance to confirm that it has entered the fractured vertebra (left). The surgeon then injects bone cement into the fractured vertebra (right), where it quickly hardens to provide stability to the bone and relief of pain.
Vertebroplasty and Kyphoplasty: Advanced procedures such as kyphoplasty and vertebroplasty allow neurosurgeons to reconstruct compressed vertebral bone, restore alignment, or remove pressure on a nerve. Vertebroplasty and kyphoplasty are image-guided procedures performed in an X-ray suite or in an operating room with X-ray equipment.
For a vertebroplasty, the patient is prone (face down) and the procedure is done either under general anesthesia or under sedation (in which the patient is awake). One or two needles are advanced under x-ray guidance into the fractured vertebra through the skin in the back. After the x-ray confirms good needle placement, the surgeon injects bone cement into the fractured vertebra. The cement hardens in a few minutes, providing immediate stability to the bone and relief of pain.
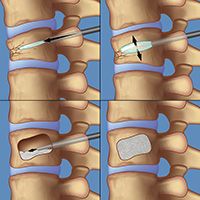
To perform a kyphoplasty, a surgeon first guides a catheter into the vertebra, then inserts and inflates a small balloon. The balloon creates a cavity as it inflates; the balloon is then deflated and withdrawn from the vertebra. In the next step, the surgeon inserts a needle into the catheter to deliver bone cement into the cavity. The cement hardens in place, providing immediate stability to the bone.
Kyphoplasty, also referred to as “balloon vertebroplasty,” is similar to vertebroplasty, but (as its name suggests) uses a balloon. The balloon is guided through the needle into the vertebra and inflated in order to correct the abnormal wedging of the broken vertebra. Once the bones are in the correct position, the balloon is deflated and removed, and the large cavity created is filled with bone cement. The cement hardens in place, providing immediate stability to the bone.
A variant of this procedure, called “structural kyphoplasty,” involves the placement of a stack of wafers instead of a balloon in an attempt to restore normal wedging. The stack of wafers is held in place with the subsequent injection of cement. Correcting the abnormal wedging may help restore the spine to a more normal alignment.
Stereotactic Radiosurgery (SRS): Neurological surgeons can use stereotactic radiosurgery (highly targeted radiation beams from multiple angles) to treat spinal tumors. This technique is a highly effective and minimally invasive treatment. Side effects are usually moderate and limited and the procedure carries a very low risk of infection or other complications that can occur after open surgery. This is a rapidly developing technique — requiring the most highly trained surgeons utilizing the most sophisticated equipment — such as the Gamma Knife, CyberKnife, proton beams, and linear accelerators — and is usually only available in major medical centers (see Doctors Who Treat Spinal Tumors).
The expert spine surgeons at Weill Cornell Medicine are fortunate to be part of the NewYork-Presbyterian Hospital team, consistently named one of "America's Best Hospitals" by US News and World Report. Our Neurology and Neurosurgery program ranks as one of the best nationwide. Together, the NewYork-Presbyterian/Weill Cornell Medical Center team is the best choice for your spine.
Reviewed by: Galal Elsayed, MD
Last reviewed/last updated: August 2024
Illustrations by Thom Graves, CMI