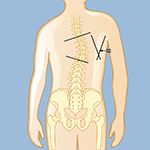
The degree of curvature is measured by drawing lines at the first and last tilted vertebrae, then drawing lines perpendicular to those lines. Where that second set of lines intersect, called the Cobb angle, is where the degree of the curve is measured.
Early detection of adolescent idiopathic scoliosis is important for successful treatment of this spinal deformity. It is important to be evaluated at an advanced spine center as soon as possible, since early and expert intervention can keep the condition from getting worse. The side-to-side spine curve of adolescent idiopathic scoliosis may be clearly visible during an adolescent’s annual check-up, and a pediatrician may be the first to refer a family to a trained orthopedic physician. In addition, many schools screen their students for scoliosis, so a school nurse may be the first to bring the condition to parents’ attention. Physical education instructors may also detect signs of adolescent scoliosis. Parents who have had other family members with the condition or who know what to look for (see Symptoms of Adolescent Idiopathic Scoliosis) may notice an excessive curve in the spine, or teens may complain that their clothing doesn’t fit right.
When adolescent idiopathic scoliosis is suspected, a trained physician will take a complete medical history and perform a physical and visual examination of the adolescent. (It is not necessary to have X-rays taken prior to consulting a pediatric spine specialist, as these will routinely be ordered by the specialist; if any early X-rays exist, however, they should be brought to the visit.)
To assess the curve, determine flexibility, and check for muscle weakness, the adolescent will be asked to stand, sit, bend over, and walk. The doctor will also check reflexes to see whether there is nerve damage.
To establish a proper diagnosis of adolescent idiopathic scoliosis and rule out other causes of spinal deformity, the physician will also want to learn:
Current physical findings and measurements will be compared to prior measurements (height, for example) and any notes on the child's spine or unusual features of other bony body parts. The doctor will look for asymmetries (uneven appearances) in the shoulders, ribs, chest, leg length, and other unusual findings, such as if the torso doesn’t appear to be evenly positioned over the pelvis, or the child’s head seems off-center.
Once scoliosis is diagnosed, there is always the question of a curve's progression. The Risser sign measures the spine’s maturity using an X-ray of an area of the hipbone (from 0-5, with 0 meaning least growth of spine and most risk of progression).
Common X-ray images taken to diagnose adolescent idiopathic scoliosis are:
If the curve pattern is not typical or if there is something unusual on the X-ray, a physician may order one or more of the following tests to provide more details:
Reviewed by: Galal A. Elsayed, MD
Last reviewed/Last updated: August 2024