
Jamie Igneri, 31, lives a pretty idyllic life these days. The special-ed math teacher lives in Manalapan, New Jersey, with her husband, Chris, and their toddler daughter. Jamie’s peaceful life is a far cry from in 2021, when a flare-up of back pain set off a tumultuous, yearlong experience that limited her movement — and her ability to hold and carry her baby girl. Thanks to some expert diagnostics and the surgical skill of Dr. Ibrahim Hussain, Jamie is back to being a mom and a teacher, pain free.

Jamie's pain started during her pregnancy
“The pain started when I was pregnant,” says Jamie, “but in my last trimester of pregnancy I started having severe pain from my lower back down to my butt. That’s how low it was. For a long time I thought it was sciatica. My husband actually has severe sciatica, and he said his symptoms were similar to mine. Even my gynecologist concurred, saying that it was likely just my baby pressing on a nerve. I dealt with the pain until I had my daughter that September. At that point, the pain suddenly went away. At least, until it suddenly came back nine months later.”
The pain was worse than it had been the first time around – Jamie describes it as being unbearable. “It shot down to my ankle and I couldn’t sleep at night — and when I could, I could only sleep upright. We still thought it was sciatica. I went to a local chiropractor in August, and they told me not to lift anything — I have a daughter, I have to lift her! They suggested hot yoga and stretches, but none of that did me any good.”
Jamie decided to take matters into her own hands, and she went to a local spine clinic, where she had an MRI. The results were surprising, to say the least: “As I was about to leave, they stopped me and said the radiologist needed to speak with me,” Jamie recalls. “That’s when they told me there was a lesion in my spinal cord, and that I needed to go to the emergency room, ASAP, to get an MRI with contrast. I was in hysterics!”
“Jamie and her husband weren’t wrong about the sciatica,” says Dr. Hussain, the neurosurgeon who eventually treated Jamie’s tumor. “It’s one of several common symptoms that present from a spinal tumor. Depending on the location, some may even develop weakness and/or numbness in the arms or legs, or experience difficulty walking or urinating. What I would advise anyone to do is, if the pain persists, to not brush these symptoms aside. You need to find their root cause — which is exactly what Jamie did.”
The MRI done at the hospital suggested that Jamie’s tumor was benign, which was good news. “The MRI showed an abnormal solid/cystic mass in the lumbar spine, suggestive of a usually benign tumor called a schwannoma,” says Dr. Hussain, “and there was severe compression of all the nerves surrounding it. This may have been growing for several months or even years.”
A benign spinal tumor isn’t cancerous, meaning it doesn’t spread into healthy tissue, but it may need to be removed to confirm it’s benign (through microscopic pathologic and genetic analysis), and if it’s causing symptoms or creating pressure on the spinal cord or surrounding nerves. In Jamie’s case, it was certainly causing symptoms. The neurosurgeon who was on call at a local hospital when Jamie when to the emergency room told her she needed surgery as soon as possible, but Jamie wasn’t so sure.
“Their approach was to remove and replace bone from my spine with metal rods. I was going back and forth — I didn’t want to have rods and all that stuff in my body at 31 years old. It was my spine, and I wanted to get a second opinion. So I decided to get one at NewYork-Presbyterian/Weill Cornell Medical Center.”

Jamie's tumor looked benign on the pre-op scan, but only pathology would know for sure
“My team and I saw things differently from the other neurosurgeon,” says Dr. Hussain, a spine specialist at Och Spine at NewYork-Presbyterian/Weill Cornell Medical Center. “We concluded that it was a slow-growing tumor that had been there for a long time, and besides the pain, Jamie didn’t have any red flag signs of numbness, weakness, or bladder dysfunction. We suspected that Jamie’s pain was related to a flare-up that could potentially be controlled with pain medication and steroids. As surgeons, we never want to jump into surgery for surgery’s sake; if we can alleviate the problem without an invasive procedure, all the better, but with close outpatient monitoring of the tumor to see if it continues to grow. On the other hand, I discussed with her that if the pain medication didn’t work, we would have a plan ready to remove the tumor – with a much less invasive approach than the first surgeon had proposed and without the need for fusion or inserting screws and rods. Jamie was young and strong enough to allow us to only shave off part of the bone if surgery were needed.”
Jamie tried the pain medications, but they didn’t seem to have any effect. “Dr. Hussain had said to call him if my pain didn’t get any better after two or three weeks,” says Jamie. “By that point, my pain had hit an all-time high, and I reached out to his office to ask about scheduling my surgery. But what I really appreciated at this point was the foresight of Dr. Hussain and his team. They told me that they’d recently had a cancellation, and Dr. Hussain had directed them to keep the appointment open for me, in case I needed the slot. That’s what makes him so phenomenal. For him to remember me and say let’s keep that appointment open and see if Jamie wants the surgery… I have nothing but good things to say about him.”
Jamie knew she had made the right decision by choosing Dr. Hussain. “Looking back, when I met him for that second opinion, he just put me at ease,” she says. “The way he talked about my surgery, and how he explained it to me, he was so knowledgeable. The other doctor had just said, ‘This is what we’re doing, and we’re doing it right away.’ They spoke in all these medical terms about cutting me open and replacing my spine with rods. Dr. Hussain, by contrast, was so comforting and empathetic.”
The day of the surgery, Jamie and her husband drove the hour and a half from Manalapan to Manhattan’s Upper East Side. They were glad Jamie was facing a less drastic procedure than the first neurosurgeon had proposed, but they were still nervous. Spine surgery may be routine for the experts, but it’s a daunting prospect for any patient. Spine tumors require a delicate surgery, with the utmost precision. And although the MRI had been informative, it didn’t show everything.
“During the surgery, which I performed with the assistance of chief resident Jacob Goldberg, MD, we leveraged some of the most advanced intraoperative technology available in the world to perform the least invasive and safest approach,” says Dr. Hussain. “We utilized special image fusion software to merge an intraoperative CT scan with low-dose radiation of Jamie’s spine with her preoperative MRI. With this image, we then used three-dimensional computer-assisted navigation guidance to target the tumor, so that I only had to remove enough bone to get to it, and without the risk of destabilization that would require a fusion with screws and rods at the same time. We knew with less than 1 millimeter of error where any object I used inside her body was in relation to the tumor.”
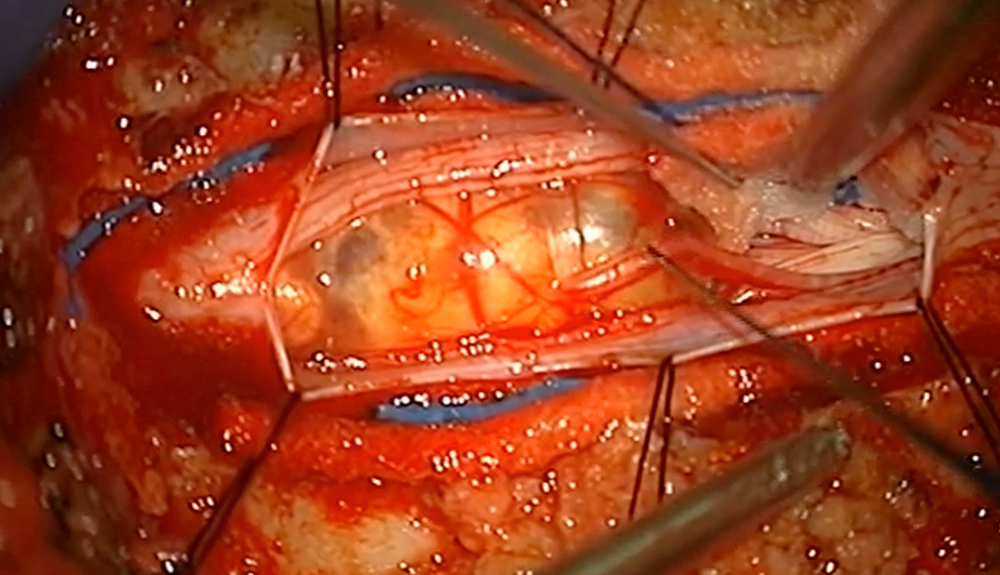
This image show's Jamie's tumor after Dr. Hussain and team opened the dura. They could clearly see the tumor adhering to and creating pressure on the surrounding nerve roots.
A team of neurophysiologists were on hand to monitor and stimulate the spinal cord and nerves during the procedure. “We also needed to determine whether the tumor lay on a motor nerve or a sensory nerve,” notes Dr. Hussain. “If it were on a motor nerve, we would have aborted the surgery, because any damage to the motor nerve would damage Jamie’s ability to move. To be safe, we’d stop and treat the tumor with radiation therapy in that situation.” Thankfully, Dr. Hussain determined using 3D navigation and neurostimulation mapping that the tumor rested on a sensory nerve, which allowed the team to proceed and resect all of the tumor.
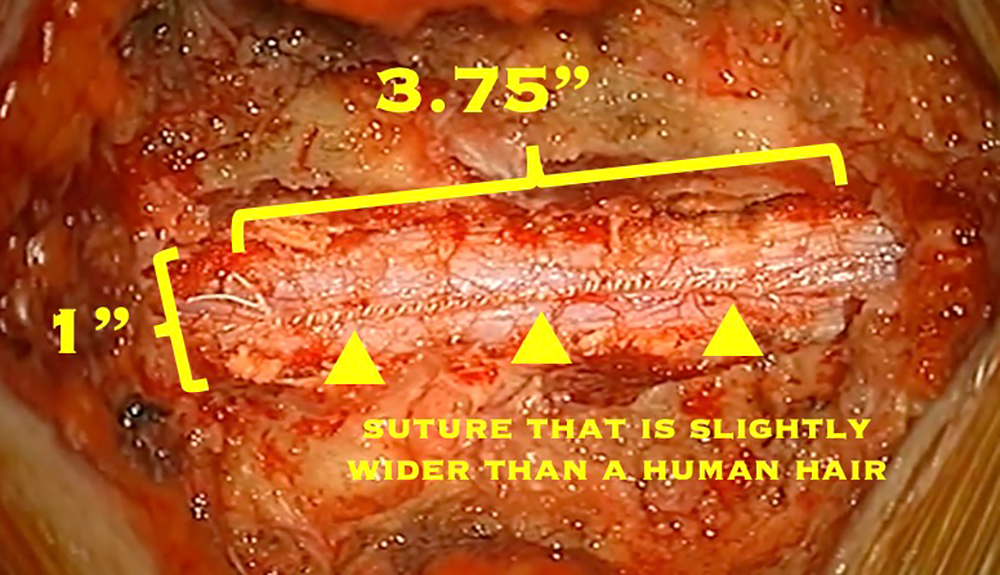
After the tumor is removed, the dura (which protects the spinal cord, nerves, and cerebrospinal fluid) must be carefully closed. Note the precise row of tiny stitches (sutures), which are just slightly wider than a human hair.

Jamie in recovery after her surgery
The surgery was a success, and Jamie was moved into a recovery room. “Dr. Hussain always came at the end of the night to check on me, no matter how late it was,” Jamie recalls. “In recovery, I had to lie flat for 24 hours — there was some spinal fluid leakage, which was drained through a tube. Dr. Hussain also warned me about severe headaches — I didn’t feel anything for the first two days, but by day three, he was right. I had horrible migraines, but at least I knew it would happen.”
Just four days later, Jamie walked out of the hospital on her own. “My husband remarked that he couldn’t believe I was walking so soon after getting spine surgery,” she laughs. “Dr. Hussain estimated that it would be six weeks to a full recovery. The hardest thing about this time was not being able to lift my daughter, who was still a baby at the time. Physically though, I was feeling way better than what I originally expected.”
Today, as Jamie spends time with her family, she’s found a deeper appreciation for life. “Before the surgery, I didn’t sleep at all. Now, I appreciate everything that I can do. There was a point where, two days before my surgery, my pain was so bad that I couldn’t take a shower on my own; my husband had to help me step into the shower. That’s how bad the pain was. I couldn’t walk. I couldn’t live a day-to-day life. I had to get the tumor removed one way or another. For anyone going through that right now, I’ll say it: spine surgery is scary — they’re operating on something that controls your entire body. But now things are better than before. I have my daughter. I’m healthy. And I can’t appreciate life more than I do now.”
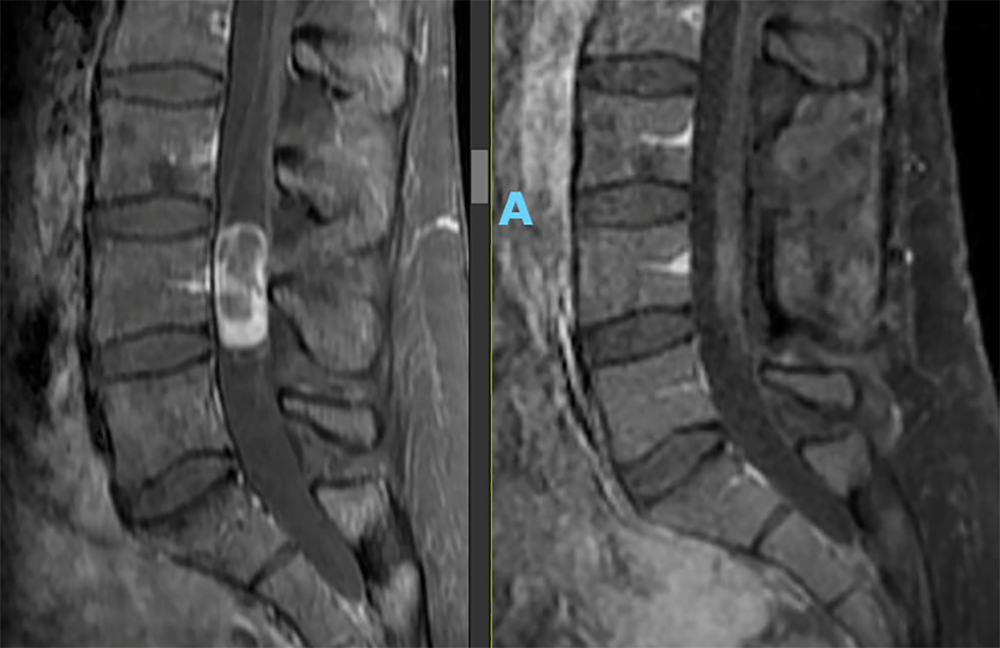
Jamie's pre- and post-operative scans show a complete resection of the tumor
More about spine surgery at Och Spine at NewYork-Presbyterian/Weill Cornell Medicine
More about Dr. Ibrahim Hussain