Sometimes surgery is required for spinal compression fractures, no matter the cause. The goal of the surgery is to fuse and repair the fracture, eliminate back pain, and restore posture and ease of movement. The most common surgical procedures for spinal compression fractures are lumbar fusion and vertebroplasty/kyphoplasty.
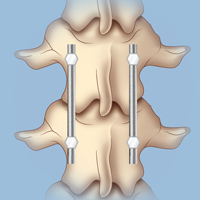
In a lumbar fusion, the vertebrae are connected with rods.
Minimally invasive lumbar fusion joins the bones of the spine in the lower back together so that there is no longer any motion between them. This procedure can repair a fracture; correct deformity; and reduce spinal pressure, pain, and nerve damage. Minimally invasive lumbar fusions do not require the large incision or the muscle retraction typically used in conventional fusions. Patients undergoing this procedure have a fast recovery time. A recent advance is the use of a computerized image guidance system for many patients undergoing lumbar fusion. This has the advantage of aiding the surgeon in optimal placement of screws and avoiding injury to delicate nerve tissue.
Until recently, all patients undergoing lumbar fusion required a bone or synthetic graft either from the hip region or from a bone bank. In most patients undergoing lumbar spinal fusion, metal titanium instrumentation is also used. This will typically involve placing pedicle screws into the bone and connecting these with a rod.
Vertebroplasty and Kyphoplasty: Advanced procedures such as kyphoplasty and vertebroplasty allow neurosurgeons to reconstruct compressed vertebral bone, restore alignment, or remove pressure on a nerve. Vertebroplasty and kyphoplasty are image-guided procedures performed in an X-ray suite or in an operating room with X-ray equipment. (Download our brochure about vertebroplasty and kyphoplasty.)
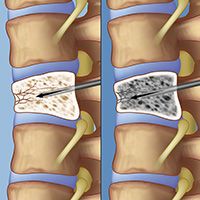
In a vertebroplasty, the surgeon advances a needle through the skin on a patient’s back under x-ray guidance to confirm that it has entered the fractured vertebra (left). The surgeon then injects bone cement into the fractured vertebra (right), where it quickly hardens to provide stability to the bone and relief of pain.
For a vertebroplasty, the patient is prone (face down) and the procedure is done either under general anesthesia or under sedation (in which the patient is awake). One or two needles are advanced under x-ray guidance into the fractured vertebra through the skin in the back. After the x-ray confirms good needle placement, the surgeon injects bone cement into the fractured vertebra. The cement hardens in a few minutes, providing immediate stability to the bone and relief of pain.
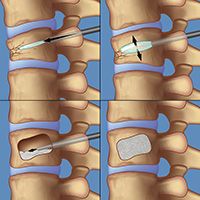
To perform a kyphoplasty, a surgeon first guides a catheter into the vertebra, then inserts and inflates a small balloon. The balloon creates a cavity as it inflates; the balloon is then deflated and withdrawn from the vertebra. In the next step, the surgeon inserts a needle into the catheter to deliver bone cement into the cavity. The cement hardens in place, providing immediate stability to the bone.
Kyphoplasty, also referred to as “balloon vertebroplasty,” is similar to vertebroplasty, but (as its name suggests) uses a balloon. The balloon is guided through the needle into the vertebra and inflated in order to correct the abnormal wedging of the broken vertebra. Once the bones are in the correct position, the balloon is deflated and removed, and the large cavity created is filled with bone cement. The cement hardens in place, providing immediate stability to the bone.
The spine surgeons at Och Spine at NewYork-Presbyterian/Weill Cornell Medical Center are fortunate to be part of the NewYork-Presbyterian team (see Doctors Who Treat Spinal Compression Fractures). We are routinely ranked as one of the top hospitals in the United States, and our Neurology and Neurosurgery program routinely ranks as one of the top programs nationwide). Together, the Och Spine at NewYork-Presbyterian/Weill Cornell Medical Center team is the best choice for your back.
Reviewed by: Srikanth Boddu, MD, MSc
Last reviewed/updated: September 2023
Illustration by Thom Graves, CMI