 Children with thalamic gliomas usually develop their first symptoms when the tumor begins to compress the adjacent ventricle, resulting in a blockage of the flow of cerebrospinal fluid (CSF). This phenomenon (also called “mass effect,” as the growth of a tumor presses against nearby brain tissue), which most commonly causes headache and vomiting, is referred to as hydrocephalus and warrants emergency attention. Tumors also commonly interfere with normal fibers surrounding the thalamus and can manifest with gait imbalance, motor weakness, or sensory disturbances.
Children with thalamic gliomas usually develop their first symptoms when the tumor begins to compress the adjacent ventricle, resulting in a blockage of the flow of cerebrospinal fluid (CSF). This phenomenon (also called “mass effect,” as the growth of a tumor presses against nearby brain tissue), which most commonly causes headache and vomiting, is referred to as hydrocephalus and warrants emergency attention. Tumors also commonly interfere with normal fibers surrounding the thalamus and can manifest with gait imbalance, motor weakness, or sensory disturbances.
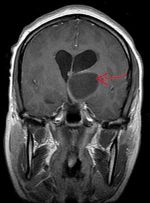
Unless a patient needs emergency treatment of hydrocephalus, the first step in investigating a suspected brain tumor is obtaining an MRI scan. The MRI provides very detailed information pertaining to the extent (unilateral or bilateral), growth character (focal or infiltrative), and potentially information on the tumor type and grade. The goal is to gather as much information as possible before treatment planning begins.
If the MRI scan indicates the tumor is a focal (clearly defined) juvenile pilocytic astrocytoma (JPA) of the thalamus, surgical removal of the tumor provides a realistic chance for a cure. Unfortunately, for most astrocytomas of the thalamus (infiltrative or diffuse Grade II-IV tumors), surgical removal is not an option. In those cases, surgery should be reserved purely for tissue sampling (biopsy), to treat hydrocephalus, or to reduce the mass effect.
Biopsy
If a biopsy is needed, an experienced neurosurgeon can usually use minimally invasive techniques, including stereotactic needle or endoscopic surgery, both of which remove small samples of a tumor through small skin and bone openings. More traditional surgery is sometimes required if a neurosurgeon is concerned about sampling error or bleeding potential.
Treatment
Like most other gliomas of the brain, thalamic gliomas are generally treated using radiation therapy with or without chemotherapy. The inclusion or choice of chemotherapy is dependent on the result of tumor biopsy. The treatment usually does not require hospitalization.
At Weill Cornell Medicine Pediatric Neurosurgery, our pediatric neurosurgeons are highly skilled in the most advanced procedures for treating rare brain tumors. Our relationships with top hospitals, including NewYork/Presbyterian and Memorial Sloan-Kettering, allow our surgeons access to the very best facilities and specialists, as well as the most leading-edge research laboratories, to ensure that each child gets the very best treatment available.
Reviewed by Umberto Tosi, MD
Last reviewed/last updated: September 2024