
When she’s on assignment, Maddie Kachurak is usually moving nonstop. The 25-year-old wardrobe stylist travels around New York and the world to work on photo shoots for advertising campaigns — sourcing clothing, developing creative concepts, and working on set to fit models. She’s more tranquil when she’s home in Brooklyn, but she’s still busy, working on her yoga practice, reading, gardening, studying herbal medicine, and volunteering at her neighborhood’s community garden. When she suddenly developed a headache, she had no reason to think she had developed a CSF leak — like most of us, she had never thought about her cerebrospinal fluid at all. It took a journey of many doctors and several hospitals to finally find a solution at the Weill Cornell Medicine CSF Leak Program at NewYork-Presbyterian.
“My life as I knew it changed one morning in December when I woke up with a headache,” Maddie recalls. “I thought nothing of it at first, but it persisted throughout the day. I figured it would go away with a good night’s sleep, but the next morning I still had it.”
The headaches didn’t go away. In fact, they got worse.
“For the first two weeks of December, I was pushing through and going to work,” Maddie says. “I’d come home from a shoot and just lie down, which gave me some relief from the pain. But when I stood back up, I started experiencing pain.”
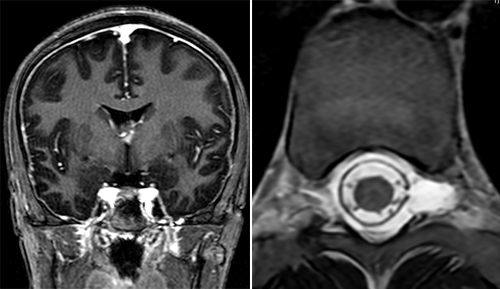
Diagnosing and treating a CSF leak requires a multi-step, multi-disciplinary approach. In Maddie’s case, the MRI scans held the first clues. Left: Evidence of intracranial hypotension in the brain. Right: An abnormal collection of fluid in the spine.
The rapid progression of symptoms worried Maddie. “A doctor at urgent care told me it was just a tension headache,” she recalls, “but it steadily got worse. I had pain in my back that left me unable to stand for more than a couple of minutes at a time. By the time the holidays rolled around I was nearly bedridden, and my primary doctor ordered an MRI. I got her call while I was on the road headed down to visit my parents in Maryland for Christmas. She advised me to go to an emergency room as soon as I arrived.” That’s when a local hospital confirmed her suspicion: a CSF leak.
“A headache is just one of the symptoms of a cerebrospinal fluid (CSF) leak,” says Dr. John Park, Co-director of the CSF Leak Program at NewYork-Presbyterian and Weill Cornell Medicine. “CSF is the fluid your brain produces to protect itself and the spinal column. If the fluid leaks, it can lead to headaches, nausea, and other neurological symptoms. Those symptoms are not exclusive to CSF leaks, however, so it can be difficult to get an accurate diagnosis. Some CSF leaks resolve on their own, but when they don’t it can be a serious, even life-threatening, situation.” (Read more about CSF leaks.)
Relieved to have a diagnosis, Maddie scheduled an appointment with a doctor in Maryland, who recommended a non-targeted blood patch. This procedure uses the patient’s blood to create a clot to stop the leak. It’s “non-targeted” when the exact site of the leak is unknown. It is less effective than targeted treatments at the leak site, but it’s often tried as a first, minimally invasive option. Maddie wasn’t satisfied.
“Dr. Salama recognized the toll this was taking on my life, and she moved things forward quickly.”
“I wasn’t getting the care I needed,” she says. “I couldn’t get hold of any of the doctors, and no one could answer my questions. I was confused about the procedure, and I didn’t have a clear path forward on how to treat my diagnosis.” Maddie turned to Google to find doctors back home in New York who specialize in CSF leaks. She found Dr. Gayle Salama and the Weill Cornell Medicine CSF Leak Program.
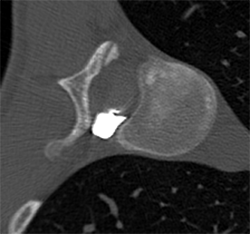
A dynamic CT myelogram identified the exact site of the CSF leak by revealing where the contrast agent had leaked.
“We brought Maddie in for an appointment as quickly as possible,” recalls Dr. Salama, Co-director of the WCM CSF Leak Program and Director of Spine Imaging and Interventions in the radiology department. “Our radiology team worked closely with colleagues in neurology and neurological surgery to create the best evaluation and treatment plan for her. That level of close collaboration among these three departments helps us deliver the highest level of comprehensive care to our CSF leak patients.”
“Dr. Salama was so action-oriented,” says Maddie. “She recognized the toll this was taking on my life, and she moved things forward quickly.”
“Through advanced CT myelogram techniques, we could see that Maddie’s CSF leak came from a tear in her dura — the protective layer around the spinal cord,” says Dr. Salama. “When the spinal dura ruptures, an interdisciplinary treatment approach results in the best outcomes.”
Dr. Salama brought in colleagues from neurological surgery (Dr. Park), neurology (Dr. Joseph Safdieh) and interventional neuroradiology (Dr. Srikanth Boddu). They couldn’t tell what had caused Maddie’s CSF leak — she doesn’t remember an injury or impact, and hadn’t had any surgical procedure, either of which can sometimes cause a CSF leak — but sometimes leaks are spontaneous, and the important thing was finding an effective solution, together.
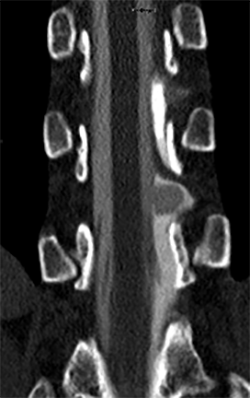
The dynamic CT myelogram also showed the CSF-filled sac protruding through the dural hole.
“Maddie needed more than one specialist,” says Dr. Park. “Dr. Salama pinpointed the location and severity of the tear, Dr. Safdieh managed her symptoms, and Dr. Boddu mapped out Maddie’s spinal arteries to ensure their safety in case surgery was needed.” Together, the team evaluated the data and came to a conclusion: Maddie was indeed going to need surgery.
“We always exhaust every option before recommending any invasive surgery,” says Dr. Salama. “An epidural blood patch, which the Maryland hospital had recommended, wouldn’t be effective in Maddie’s case. Our imaging showed that the hole in her dura was too large to be patched, leaving open surgery as the only option on the table.”
“When I heard about the need for surgery, I was so overwhelmed,” recalls Maddie. “I’d never had any health problems, so this was very new to me. I hate needles, blood, and hospitals! But all my doctors were amazing. It was such a contrast to the previous hospital. Not only did I feel heard and validated, but I also felt confident in their care. I felt like they were communicating about my case and that they were working together to figure out the best course of action. I was thankful to be able to reach them all with ease, get insight, and schedule appointments when needed.”
Maddie understood that there was one big unknown going into surgery. “We didn’t know how much spinal bone we’d have to remove to get to the leak,” says Dr. Park. ”Once you remove a certain amount of bone, the spine needs to be stabilized with metal rods, and you don’t know that in advance. Thankfully, we were able to suture the leak without removing too much bone, and no rods were needed.”
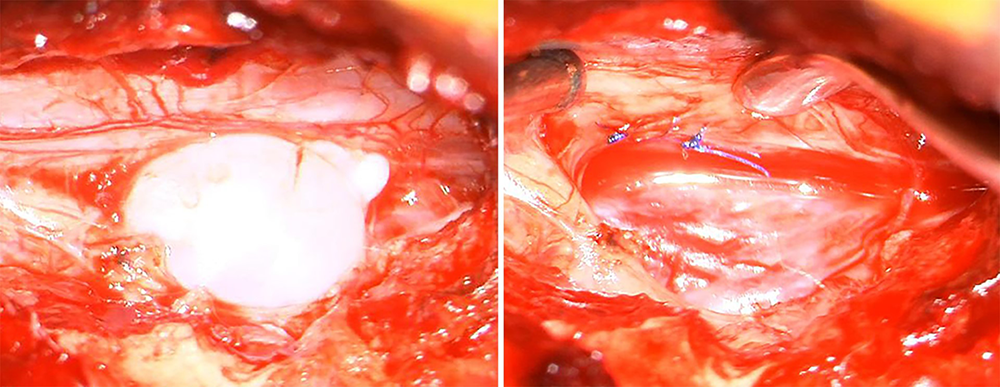
These photos of Maddie’s surgery show the out-pouching of the CSF-filled sac through the tear in the dura (left) and the operative results after the sac was removed and the tear in the dura sutured (right).
The team helped Maddie through her recovery period as she built back her strength and managed through the predicted “rebound headaches” after surgery. “I met with Dr. Safdieh, who worked with me to adjust my medication as the headaches faded over time,” she says. “Dr. Salama continually emailed me to check up on me after surgery.”

Maddie Kachurak is back to living her active life
Today, Maddie feels completely healed. “I was in tears the first time I was able to do yoga again,” she says. “For a long time I didn’t feel like myself. But now, my body is back to where it used to be before all this happened. I listen to my body so much more, and I trust what it’s telling me. I used to work very long hours on my feet, pushing my body, but now I always take time for rest. I don’t take even the simplest activities for granted. Being able to stand up and cook a meal is a blessing to me.”
Maddie has advice for anyone facing a CSF leak: You are so much stronger than you know!
“This was scary,” she says, “but you are in good hands at Weill Cornell Medicine and you can get through this. You will have your life back again, no matter how far off that might seem at the moment.”
More about the CSF Leak Program at Weill Cornell Medicine and NewYork-Presbyterian