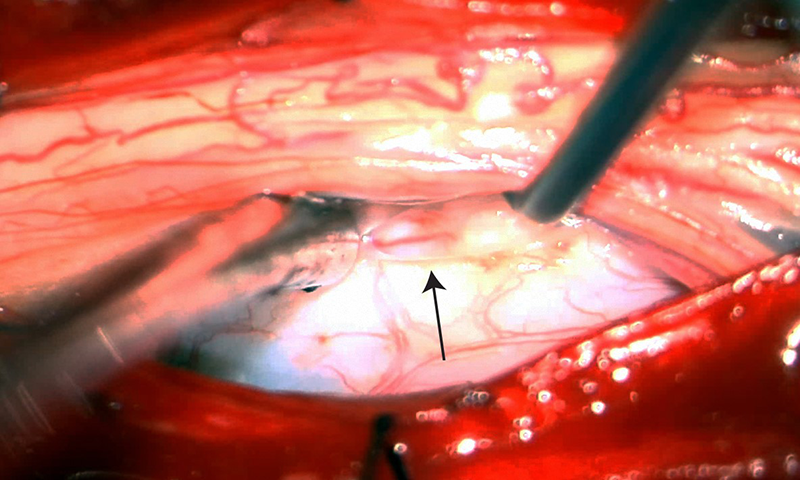
Photo from a surgery repairing a spinal dural tear (arrow) caused by a bone spur.
CSF leaks occasionally resolve on their own with conservative therapies such as bedrest, caffeine, increased fluid intake, and pain medications, which can be tried for one to two weeks. If bed rest and other conservative treatments fail, an expert in CSF leaks may recommend one of the following approaches:
Treatment for spinal CSF leaks
An epidural blood patch (EBP) or epidural fibrin patch (EFP) is often the first treatment for a spinal CSF leak. An EBP, which uses the patient’s own blood, can be applied at the location of the leak if known (targeted), or in the lower back when the leak location is unknown (nontargeted). An EFP is used for targeted treatment when a leak location is identified. Epidural patches can be effective for symptom management for CSF leaks in any spinal location, or even in cases where the source cannot be identified. It may take several treatments to resolve the leak. If EBPs or EFPs are not effective and the location of the leak is known, surgical repair or venous embolization are often performed. Surgery is typically used for a leak caused by a tear in the dura, when fluid is leaking into the body cavity. Embolization can be used for CSF-venous fistulas, in which the CSF is leaking into an adjacent blood vessel. The embolization procedure is done through an incision in the leg; the surgeon threads a catheter to the site of the fistula and uses a kind of glue to repair the fistula.
Treatment for cranial CSF leaks
For cranial leaks, a neurosurgeon experienced in the treatment of CSF leaks will likely recommend surgical repair. The surgical repair is made at the site of the leak and involves plugging the hole in the dura using a special sealant. The extent of the surgery depends on the location of the leak. Leaks that can be reached through the nostrils may be repaired using an endonasal approach, while leaks in other locations may require open surgery. Sometimes patients will also require a lumbar drain, which helps divert CSF leak away from the primary dural hole and allows for healing.
Reviewed by: Gayle Salama, MD, and John Park, MD, PhD
Last reviewed/last updated: February 2023