Vertebroplasty and kyphoplasty are image-guided procedures performed in an operating room with x-ray equipment. Both vertebroplasty and kyphoplasty are successful about 80 to 90% of the time in relieving the pain of fractured vertebrae. Both procedures involve the injection of a polymer (“bone cement”) into the fractured bone. This not only provides pain relief, but also stabilizes the bone and prevents progression of the fracture and associated kyphosis, an abnormal curvature of the spine.
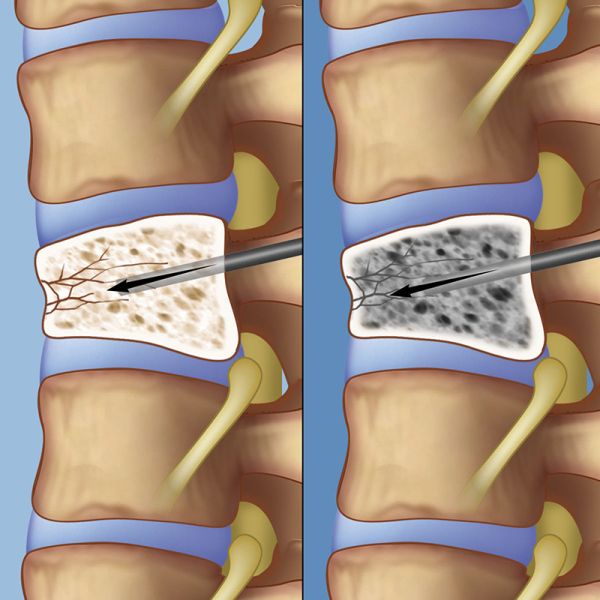
In a vertebroplasty, the surgeon advances a needle through the skin on a patient’s back under x-ray guidance to confirm that it has entered the fractured vertebra (left). The surgeon then injects bone cement into the fractured vertebra (right), where it quickly hardens to provide stability to the bone and relief of pain.
Both procedures are performed with the patient in a prone position (face down). We typically perform these procedures with local anesthesia and sedation (“twilight” anesthesia, similar to colonoscopy). Only rarely is general anesthesia required. Both procedures involve the careful advancement of one or two needles under x-ray guidance into the fractured vertebra through very small incisions in the back. The x-ray guidance is essential to allow us to position the needles safely in the bone while avoiding sensitive parts of the body such as nerves.
After the x-ray confirms good needle placement, the surgeon injects bone cement into the fractured vertebra. The cement hardens in a few minutes, providing immediate stability to the bone and relief of pain. Kyphoplasty, also referred to as “balloon vertebroplasty,” differs slightly from vertebroplasty, as it involves the extra step of balloon inflation in the fractured bone in order to correct the abnormal wedging. The balloons are then removed and the cement is infused as in a vertebroplasty. After the procedure the patient remains in the recovery area for two to three hours before being discharged to home.