Thanks for testing your brain and spine smarts! Now let’s find out how you did:
1. What part of your brain controls basic functions such as breathing, swallowing, and consciousness?
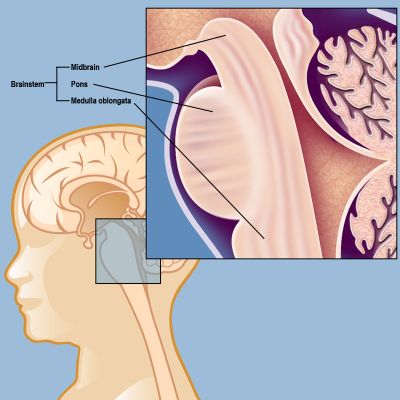
The correct answer is c: the brain stem
The cerebral cortex is what is commonly referred to as gray matter — it’s the folded layer, packed with neurons, around the cerebrum. Synapses are the gaps between those neurons, the spaces across which signals are transmitted from one part of the brain to another. The brain stem, however, is the most primal region of the brain — the part responsible for our very survival. It connects the brain to the spinal column, so all the signals from the brain to the rest of the nervous system pass through this important structure. The brain stem also controls breathing, heartbeat, balance, swallowing, and the sleep/wake cycles.
A tumor in the brain stem is an extremely serious diagnosis, since the area is so delicate that it is often impossible to approach surgically. One such tumor, called Diffuse Intrinsic Pontine Glioma, occurs primarily in children under 10 and is universally fatal. The Children’s Brain Tumor Project at Weill Cornell Medicine is one of the foremost research centers in the world studying DIPG and other rare and inoperable brain tumors of childhood and adolescence. (Read more about DIPG and the Children’s Brain Tumor Project.)
2. What are the two most common reasons for a doctor visit in the United States?
The correct answer is b: colds and back pain
A quarter of all American adults experience back pain each year, and millions of them go to the doctor for it, second only to coughs and colds. The good news is that back pain is very often caused by muscle strain, which usually requires no treatment other than ice or heat, anti-inflammatory medications, and a few days of recovery time. If back pain doesn’t respond to these simple measures after four to seven days, a doctor’s visit is in order.
For those individuals whose back pain does require medical care, some of the most common diagnoses are herniated disc, spinal stenosis, and compression fractures. But there are other conditions that might be present, so an accurate diagnosis is critical to developing an effective treatment plan. A multidisciplinary team approach ensures that each patient gets the best therapies, whether they need pain management, physical therapy or other rehabilitation medicine, or surgery.
At Och Spine at NewYork-Presbyterian at the Weill Cornell Medicine Center for Comprehensive Spine Care, we offer a comprehensive range of treatment options for back and neck pain. If surgery is part of the treatment plan, our internationally renowned experts in minimally invasive techniques can get you back on your feet with less pain, faster recovery times, and less scarring than was typical of older, open surgeries. Find out more about our Back and Neck Pain Program at our spine center.
3. How many Americans suffer a stroke each year?
The correct answer is b: nearly 800,000
Nearly 800,000 individuals in the United States experience a stroke, or “brain attack,” each year. Stroke is the fifth-leading cause of death in the United States and the second most common cause of neurological disability (after Alzheimer's disease). Strokes are serious neurological emergencies that need to be treated immediately.
Approximately 80 percent of all strokes are ischemic strokes, caused by the blockage of a brain artery. Risk factors for these blockages include high cholesterol, high blood pressure, diabetes, smoking, and obesity. A mild ischemic stroke can be treated with intravenous administration of t-PA, a clot-dissolving medicine, when it is given within about four hours of symptom onset. More significant blockages may be treated with mechanical embolectomy, in which a surgeon inserts a microcatheter (a small plastic tube) into the artery in the patient’s upper leg and threads it (under X-ray guidance) into the blocked artery of the brain. The surgeon then slips a device inside the plastic tube and advances it to the site of the clot to aspirate (remove) the clot.
The Weill Cornell Medicine INR (Interventional Neuroradiology) team is highly experienced in endovascular stroke treatment, having developed the first-ever mechanical embolectomy device 15 years ago and having initiated or participated in most of the major clinical trials on treatment of acute ischemic stroke.
Find out more about the Stroke Program at Weill Cornell Medicine Neurological Surgery, and the designation of NewYork-Presbyterian/Weill Cornell Medicine as a Comprehensive Stroke Center.
4. What injury can often be prevented by wearing a helmet while bicycling?
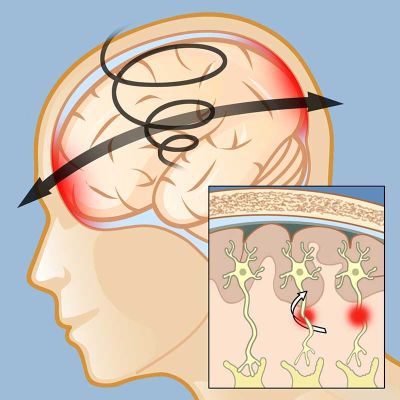
The correct answer is b: skull fracture
Many people think a bike helmet protects against concussion, but the real reason for wearing one is to keep the skull from fracturing in the event of an accident. A fracture can damage the blood vessels within the skull, disrupt the flow of cerebrospinal fluid, and lead to dangerous bleeding in the brain. Preventing a skull fracture is the number one reason to wear a helmet during contact sports, and for parents to insist on helmets during bike rides.
What a helmet won’t do is stop the brain from striking the inside of the skull or from rotating within it. As shown in this illustration, a concussion causes injury in two places, where the brain strikes the inside of the skull at the point of impact and then again on the opposite side as it rebounds away from the impact site. If the head rotates at the time of impact there can also be damage to the axons that connect the brain's gray matter to the white matter below (inset).
Concussion is a “functional” brain injury, not a “pathological” one. That means it’s a real injury that affects how the brain works, but the effects are usually temporary. Concussions usually resolve on their own within one to six weeks without medical treatment. They do require a patient’s cooperation, though: The brain needs rest, both physical and cognitive, in order to recover. A trained clinical neuropsychologist can assess the patient and make a recommendation on how much time will be needed to allow for a full recovery. The neuropsychologist can also identify any post-concussion difficulties that do require intervention.
5. What part of the body is reacting when you experience “brain freeze” or "ice cream headache"?
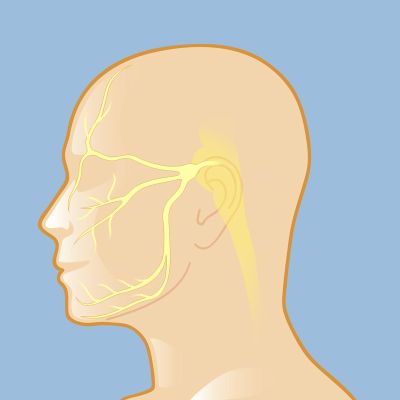
The correct answer is a: the trigeminal nerve
It’s happened to almost all of us — take a too-fast slurp of a frozen drink and a searing pain fires across your cheek. That would be your trigeminal nerve, the fifth cranial nerve, which transmits signals between the brain and the face, eyes, and teeth as well as the muscles that control chewing. There are two trigeminal nerves, one on each side of the face, and each has three branches: the ophthalmic nerve, the maxillary nerve, and the mandibular nerve.
Most of us experience the pain of an irritated trigeminal nerve only fleetingly, but for individuals with trigeminal neuralgia the pain can be disabling. Trigeminal neuralgia (also known as TN, or tic douloureux) is a chronic condition that causes intense facial pain, usually down one side of the face. It most commonly develops in those over 50, particularly women, but it can occur in younger people and men as well. TN can affect any of the three branches of the trigeminal nerve, but it most commonly affects the maxillary and mandibular nerves.
TN can often be treated with anti-spasmodic, anti-epileptic (anticonvulsant), and tricyclic anti-depressant drugs, since these quiet hyperactive nerves and dull pain signals from the trigeminal nerve. Patients sometimes try complementary and alternative medicine (CAM) approaches, including acupuncture, acupressure, vitamin therapy, and electrical stimulation of the nerves.
For some patients these treatments are insufficient, or they become ineffective over time. Those patients may consider surgical options for trigeminal neuralgia, including microvascular decompression, stereotactic radiosurgery, deep brain stimulation, or rhizotomy. (Find out more about Surgery for Trigeminal Neuralgia at Weill Cornell Medicine Neurological Surgery.)
 6. Which of the following may contribute to a herniated disc?
6. Which of the following may contribute to a herniated disc?
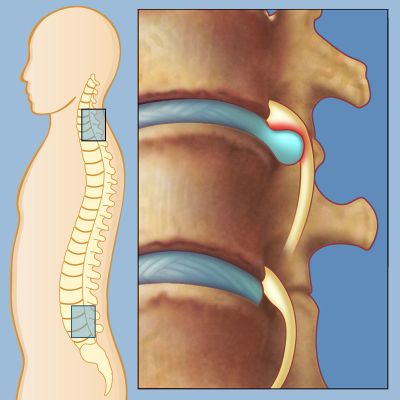
The correct answer is c: either age or injury
A herniated disc, also called a slipped disc or ruptured disc, can occur from excessive strain or injury, or degeneration due to age. It can happen in any part of the spine, but is most common in the lumbar (lower back) or cervical (neck) regions. A disc is said to herniate when its nucleus (the soft center of the disc) bulges out of its tough covering (the annulus). The bulge puts pressure on the nerves, and it’s that pressure that causes pain.
A few preventive measures can help keep discs from herniating, or keep a herniated disc from recurring:
Most patients with a herniated disc will make a full recovery after treatment, and if surgery is necessary our experts have advanced minimally invasive options to get you back in action quickly. (See Diagnosing and Treating a Herniated Disc.)
7. What is the most common cancer diagnosed in children?
The correct answer is a: leukemia
Barely a generation ago, a child diagnosed with leukemia had an extremely grim prognosis. Today, thanks to decades of research, the most common type of leukemia (acute lymphoblastic leukemia, or ALL) has a survival rate better than 90 percent. Researchers continue to search for effective treatments for ALL and other, more aggressive forms of the disease, but the tide has turned and most children with leukemia are expected to be cured.
Unfortunately, the last few decades did not bring similar advances in the second most common type of cancer in children, which are cancers of the central nervous system. Brain tumors in children are especially deadly, with many of them inoperable and others too rare to justify major research funding. Tumors that are rare and inoperable, including invasive tumors such as DIPG and gliomatosis cerebri, remain almost universally fatal.
Since “only” a few hundred children a year are diagnosed with these tumors, the federal government and large funding agencies don’t generally support research to find cures for these tumors. Although it’s understandable why funding gets directed to common conditions, where advances help thousands of patients, it’s unacceptable that hundreds of children die each year because of a lack of research into their rare tumors.
The Weill Cornell Medicine Children’s Brain Tumor Project is a research effort that is funded almost entirely by families and communities of children diagnosed with brain tumors. These families know all too well what’s at stake, and that even one child is one too many to lose. Funding from these private donors has allowed us to create a world-class laboratory making progress against these terrible tumors. Find out more about the Children’s Brain Tumor Project.
8. Which factor has the most important effect on your odds of surviving a stroke?
The correct answer is b: the type of stroke
Both age and access to medical care have large impacts on the odds of surviving a stroke, and surviving it with good quality of life. An older patient, or one who is far from a Comprehensive Stroke Center (such as NewYork-Presbyterian/Weill Cornell Medicine), is at much greater risk of death or disability from a stroke than one who is younger and closer to expert care.
The type of stroke someone has, however, makes the biggest difference in how the patient is treated and what the odds of survival are. Only 10 to 15 percent of strokes are hemorrhagic strokes, meaning strokes caused by bleeding in the brain, but they carry a much higher risk of death or disability, with some studies showing a nearly 40 percent fatality rate in the immediate aftermath of the stroke. One recent study reported less than 30 percent of hemorrhagic stroke patients surviving five years after the event. And many of those who do survive a brain bleed do so with significant neurological impairments.
An individual suffering an ischemic stroke, on the other hand, has a good chance of survival and recovery if treatment is provided quickly. For those experiencing an ischemic stroke, which is caused by a blockage in the blood vessels that oxygenate the brain, access to a health care facility that can administer the clot-busting drug tPA can vastly improve the odds of survival. In some cases, advanced embolectomy (the mechanical removal of a small clot deep in the brain) can help restore good blood flow and prevent the brain damage caused by lack of oxygen.
The neurosurgeons and interventional radiologists at Weil Cornell Medicine Neurological Surgery have additional expertise in cerebral neovascularization, also called bypass surgery, which is used to address “cerebrovascular insufficiency,” or a reduction in oxygen to the brain due to a blocked or narrowed carotid artery. Cerebrovascular insufficiency can lead to a stroke or a transient ischemic attack (TIA or "mini-stroke"), so cerebral neovascularization surgery provides new blood supply that can help prevent strokes and TIAs.
Find out more about Cerebrovascular Neurosurgery at Weill Cornell Medicine.
9. How can epilepsy be treated?
The correct answer is b: medication or surgery
A seizure is an electrical disturbance in the brain; about 10 percent of people will experience one at some point during their life, often after an accident or other traumatic injury. During a seizure normal electrical patterns in the brain become disrupted and can cause anything from unusual sensations and behaviors to convulsions, muscle spasms, and loss of consciousness. When seizures are recurrent, the person is said to have a seizure disorder, or epilepsy.
Epilepsy can develop suddenly in anyone of any age, and it is most common in young children and in the elderly, and in those who have suffered traumatic brain injuries (such as veterans returning from combat). Many individuals with epilepsy can achieve good control of their seizures using anti-epileptic medications, but others cannot. For some patients whose seizures do not respond well to medication, there are surgical procedures that may control or even cure epilepsy.
In some patients, doctors can locate the precise area of the brain where a seizure begins. In these individuals, cranial implants that can be programmed to disrupt abnormal activity in the brain as soon as it begins can prevent a seizure from spreading. (See one patient’s story of how an implant changed her life.)
Some patients may be candidates for surgery to actually remove that tiny spot in the brain where seizures begin, effectively curing their epilepsy. Neurosurgeons who have developed expertise in epilepsy surgery have advanced new options for this procedure, including a minimally invasive laser ablation. (Read more about this new laser surgery.)
Find out more about the Epilepsy Surgery Program at Weill Cornell Medicine.
 10. What is the most common symptom of a brain aneurysm?
10. What is the most common symptom of a brain aneurysm?
The correct answer is c: nothing
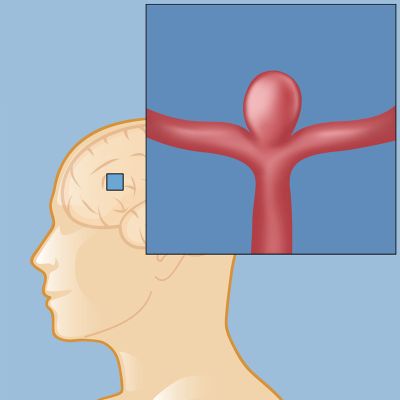
An aneurysm develops as a weakness in the wall of an artery; the pressure from blood flowing past the weak point causes the artery to swell at that spot. The resulting bulge is called an aneurysm, and it’s entirely possible to have one without knowing it. In the diagram at right, a berry aneurysm (the most common type) has developed where a large artery branches into two smaller ones.
The real risk of having an aneurysm is that it may one day start to leak or rupture without warning. Symptoms of a leak or rupture can come on suddenly and be quite severe, including a “thunderclap headache,” nausea and vomiting, neck pain, a sense of disorientation, and vision changes. A leaking or ruptured aneurysm requires immediate treatment before bleeding into the brain leads to damage or even death.
Not long ago, a rupture was often the only way an individual would find out he or she had a brain aneurysm. Today more and more people are diagnosed incidentally, when a scan performed for another reason (such as after a car accident or other traumatic injury) reveals the presence of an aneurysm.
When an aneurysm is found, an expert in cerebrovascular conditions should evaluate it in order to make a recommendation on whether or not to treat it. Small aneurysms that are not causing symptoms may not be at high risk for rupture, and a neurosurgeon may recommend a wait-and-see approach with regular scans to monitor the aneurysm for any changes. An aneurysm that is larger, causing symptoms, or located in the posterior (back) of the brain is often judged a greater risk for rupture, and surgery may be recommended. Since the consequences of a rupture can be catastrophic, a patient whose aneurysm is judged to be at risk for rupture is very often referred for surgery.
To repair an aneurysm, cerebrovascular neurosurgeons can now choose from a few different options based on the patient’s needs. Clipping and coiling, or a combination of the two, are the procedures most often performed to correct an aneurysm. Find out more about repairing an aneurysm, and read this story of an innovative use of a stent on a patient with a particularly difficult case.