
At 56, Edwin Gonzalez could still hold his own on the basketball court. Ed is the head coach of the boys’ varsity team at Bishop Loughlin Memorial High School in Brooklyn, where he is also director of admissions. “Sometimes I would shoot hoops with the team,” he laughs, “and even though they’re the ones playing, I could still show them a thing or two!” Life changed very suddenly for Ed one day, but thanks to quick work by Dr. Ning Lin and the team at NewYork-Presbyterian Queens, he’s on his way back to his best form.
Ed’s humor was always well known, but his dedication to his work is intense – he says that he, like his team, always gives 100 percent. “Games needed to be played and the players needed to be attended to,” Ed says. “It was hectic!” His wife, Joyce, saw the toll this took on him. “Many nights when arriving home, he’d complain of headaches,” Joyce says. “But he thought it was from not eating enough... he would just pop an ibuprofen and go to bed.” Little did they know that those headaches were warning signs of an aneurysm about to rupture – which happened on the night of Bishop Loughlin’s first game of the season.
Bishop Loughlin was playing an away game at St. Francis Prep in Queens that night. With just over a minute left on the game clock, the assistant coach saw Ed sit down — something Ed never did. “At the time I felt a bit dizzy and lightheaded,” Ed recalls. “The assistant coach told me that my eyes rolled behind my head… and I guess that’s when I passed out.” Medical staff on hand for the game administered first aid until an ambulance arrived to rush Ed to nearby NewYork-Presbyterian Queens, where emergency room staff took a CT scan.
Dr. Ning Lin was on call for neurosurgery that night and saw Ed in the emergency room. After taking a look at the CT scan, Dr. Lin immediately recognized the danger. "Ed had subarachnoid hemorrhage from a ruptured cerebral aneurysm,” he explains. “An aneurysm is like a bubble outside a blood vessel wall. If the bubble bursts, it can cause very serious bleeding, which is associated with high likelihood of disability and even death. A ruptured aneurysm requires emergency treatment to eradicate risks of re-rupture.” A specialist in cerebrovascular emergencies like this one, Dr. Lin knew that an immediate embolization procedure was needed to prevent bleeding from happening again.
As soon as the family got the call about Ed’s condition, his children rushed to be by his side while the rest of the family awaited his transfer to Manhattan that night. "I'm very proud of the decisions the kids made at the moment of the injury and for how his entire staff stood by for support," recalls Joyce. "We would have never imagined how our lives were about to change, with the instant routine of our round-the-clock bedside visits and taking turns being there for him. We're a strong family — it’s just what we do!"
Joyce later recalled, “Ed was so out of it that he didn’t know his diagnosis until after the procedure. Dr. Lin told me that he was stable, but there would be some road blocks for his recovery.”
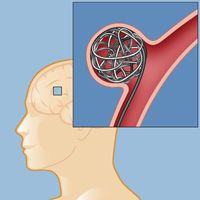
Aneurysm surgery: coiling is a minimally invasive procedure done from inside the blood vessel, no open brain surgery required.
Ed was transferred emergently to NewYork-Presbyterian/Weill Cornell Medical Center, and the aneurysm embolization was performed next day. Dr. Lin utilized a catheter to access the aneurysm and filled the bubble with small platinum coils. (This minimally invasive coiling method requires no open surgery, as the aneurysm is reached from the inside.) Even after the aneurysm was successfully treated, Dr. Lin and his team kept a vigilant eye on Ed. The original bleed can lead to serious medical complications, and for two weeks Ed was monitored in the neuro-intensive care unit for something called cerebral vasospasm. “It’s a condition that we see frequently in patients with high-grade subarachnoid hemorrhage,” says Dr. Lin. “When there is blood in the brain, the normal blood vessels can be irritated and become smaller in size. This can cause confusion, mental status change, and in severe cases even strokes.” Throughout this period, Ed was treated carefully in the neuro-ICU, and after 14 days, he was finally in the clear.
With that crisis averted, Ed faced another problem: hydrocephalus — a buildup of cerebrospinal fluid (CSF) in the brain. CSF is the fluid that assists in nourishment, protection, and waste removal from the brain and spinal cord, and normally it regulates itself. When it doesn’t drain properly, however, the buildup of excess CSF puts pressure on the brain. “The blood from the aneurysm rupture also blocked the circulation of CSF,” says Dr. Lin. “As a result, there was more CSF being produced than was absorbed by the body.” Ed would need a shunt to restore the balance and relieve the pressure on his brain. “This surgery is routine,” says Dr. Lin. “We insert a catheter into the ventricle to divert the CSF out of the brain, and connect it to a catheter into the abdominal cavity. The shunt relieves pressure on the brain by moving the excess CSF to the abdomen, where it is absorbed by the peritoneum into the body.”
Ed Gonzales
After the surgery, it looked like the worst was over. “When I saw him in the recovery room, it was as if he was there for a routine visit!” recalls Joyce. “He was conscious, alert, and just lying in the bed waiting to return to his room. It was amazing — and we were transferred that night. From there, it was a quick ride out of the hospital and into rehab a week later.”
According to Dr. Lin, several factors worked in Ed’s favor. “Thankfully, he got to the hospital early and his neurological status was relatively good. We were able to embolize the aneurysm right away, and he got excellent care from the ICU team. His baseline health was also very good to begin with. All these things contributed to his good eventual recovery."
Physical rehabilitation proved to be a challenge after being bedridden for a month. “I had to learn to walk again and gain my strength overall,” says Ed. He made great strides at inpatient rehab, but then it all had to be put on hold due to the coronavirus outbreak. “It put a damper on my momentum — I was working towards the finish line, and lacking the therapy has taken a bit of a toll on me. I am, however, working out at home virtually and doing the best I can on my own,” he says.
Ed and Joyce remember well the glimmers of joy they experienced throughout the journey. “There are so many stories we can share,” says Joyce. “One moment of light was, after spending the holidays in the hospital, we fed the entire staff a Christmas dinner as our way of thanking them for all that they were doing for him. He wants to visit them again once the pandemic is all over to personally thank them. That’s just who Ed is!”
Although the coronavirus pandemic put Ed’s therapy on hold, it also made it easier for him to get in touch with everyone while he recovers. He’s been working directly with Bishop Loughlin’s administration once a week and communicating with parents for incoming student admissions. “The staff, students, and parents have been overwhelmingly supportive in every way possible,” Ed says. “I’m thankful and grateful to be a part of an organization that has been by my side every step of the way — they truly showed me that we are not just co-workers, but a family!”
For anyone else who finds themselves in a similar place, Ed cautions against the lifestyle he led before his aneurysm. “To all those people living a busy lifestyle, listen to your body! There’s nothing more important in life than your own life. Don’t self-diagnose and try to guess what may be wrong — leave that to the professionals. And if you find yourself with the same condition, put your faith in God and let Dr. Lin do the rest!"
2021 Update: Coach Gonzalez is back!