Diffuse intrinsic pontine glioma (DIPG) is one of the most challenging pediatric brain tumors to treat due to its location in the brainstem and resistance to conventional therapies. However, a groundbreaking clinical trial led by Dr. Mark Souweidane, director of pediatric neurological surgery at Weill Cornell Medicine and NewYork-Presbyterian, offers new hope.
Dr. Souweidane and his research team at Weill Cornell Medicine’s Children’s Brain Tumor Project have been at the forefront of developing a novel drug delivery technique known as convection-enhanced delivery (CED). This approach bypasses the blood-brain barrier by infusing drugs directly into the brainstem, ensuring higher drug concentrations reach DIPG tumors.
The phase 1 clinical trial, conducted in collaboration with Memorial Sloan Kettering Cancer Center, demonstrated that CED is both safe and effective in distributing treatment throughout DIPG tumors. Traditionally, the median survival for children diagnosed with DIPG is 8 to 12 months, but several participants in this trial have surpassed three years post-treatment—a significant milestone in the field.
"This is the most exciting thing I’ve done in my career by far," said Dr. Souweidane. “I’ve been in this for 30 years, and you just watch these kids die with no alternative. It’s constant, constant turmoil and tragedy. It’s amazing to think you’re on the verge of something big.”
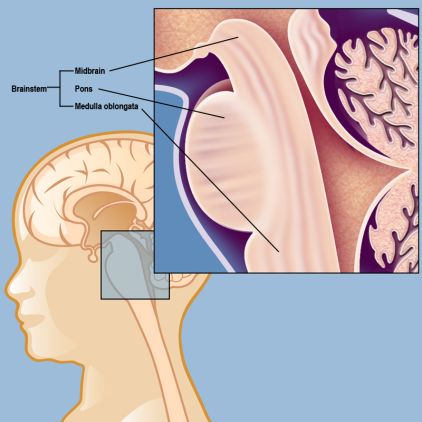
The brainstem consists of three parts: The midbrain, the pons, and the medulla oblongata. DIPG is a pontine glioma, meaning that it develops in the pons.
CED involves implanting tiny catheters deep into the brainstem and delivering therapeutic agents over 12 hours. This controlled infusion allows the drug to spread through the tumor more effectively than conventional methods. The study also revealed that drug concentrations in tumors were up to a thousand times higher than levels achieved through traditional systemic delivery.
Previously, CED had been tested primarily on adult brain tumors, such as glioblastoma, another aggressive cancer. Dr. Souweidane says the drug delivery technique is better suited for DIPG because these tumors are smaller and restricted to a tighter area.
These promising results pave the way for further research into refining CED for DIPG and potentially other hard-to-treat brain tumors. Dr. Souweidane and his colleagues continue to explore optimal dosing strategies and imaging techniques to enhance treatment outcomes.
This research was made possible through the support of numerous foundations, including the Cristian Rivera Foundation, McKenna Claire Foundation, The Lyonhearted Foundation, Christian Koehler Foundation, Brooke Healey Foundation, Fly a Kite Foundation, Children’s Brain Tumor Family Foundation, Joshua’s Wish, Lily LaRue Foundation, and Alex Lemonade Stand Foundation for Childhood Cancer.
This story was adapted from an article originally published on the Memorial Sloan Kettering Cancer Center newsroom.
We thank our collaborators at MSK for their vital contributions to this study.
The results are published in Neuro-Oncology.